ms symptoms but normal mri
 Imaging in multiple sclerosis | Journal of Neurology, Neurosurgery & Psychiatry
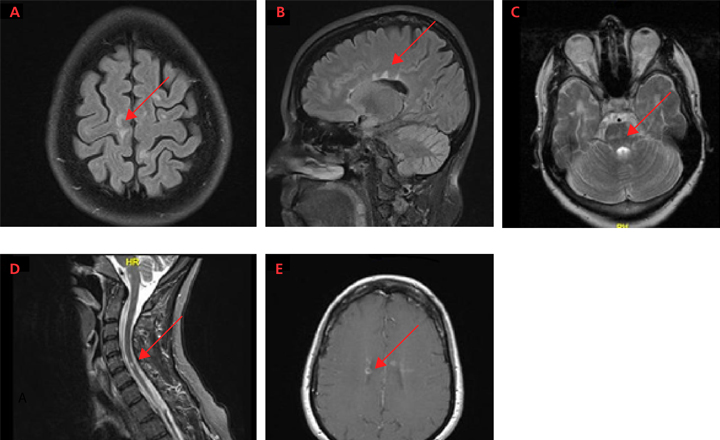
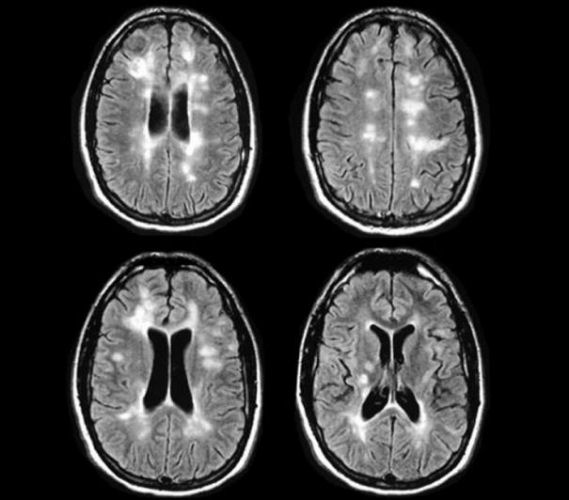
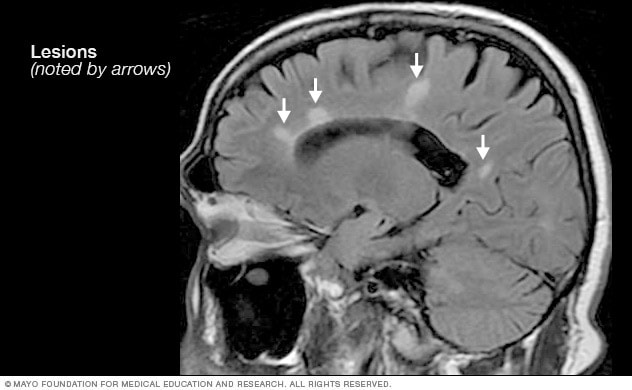
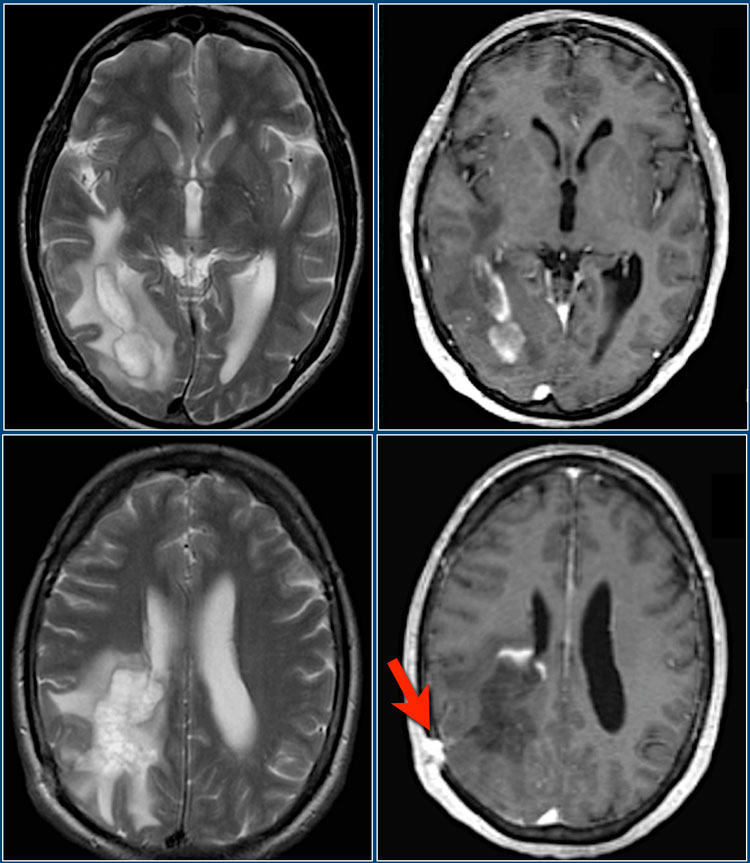
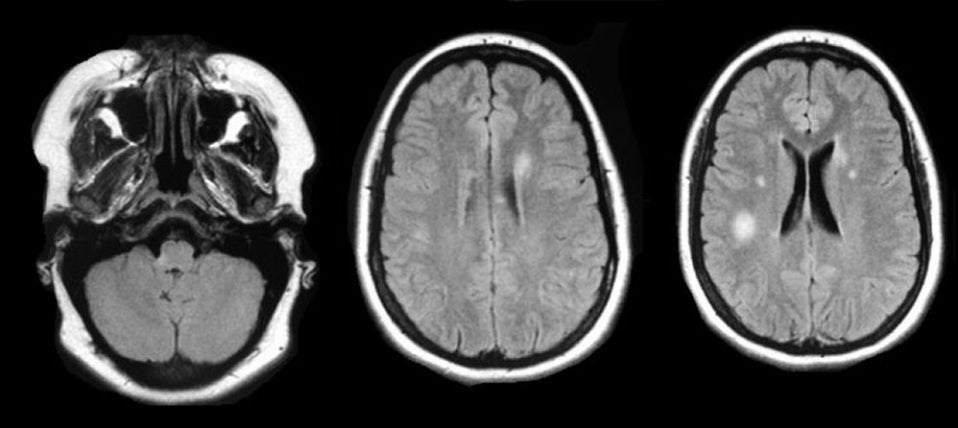
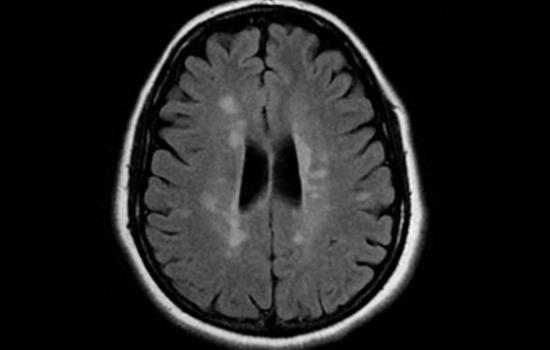
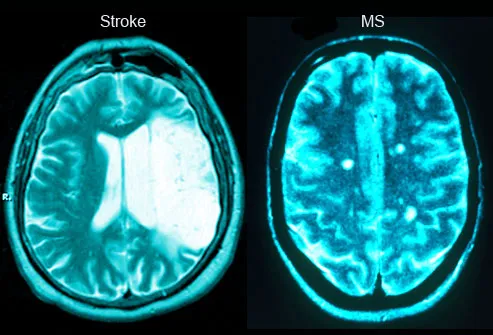
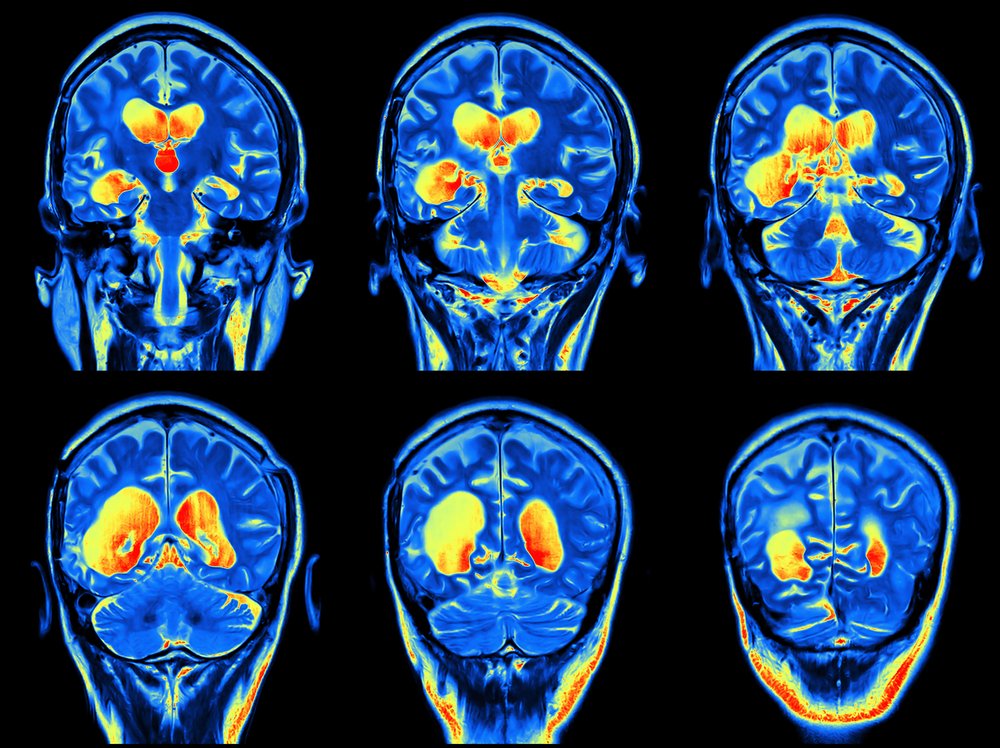
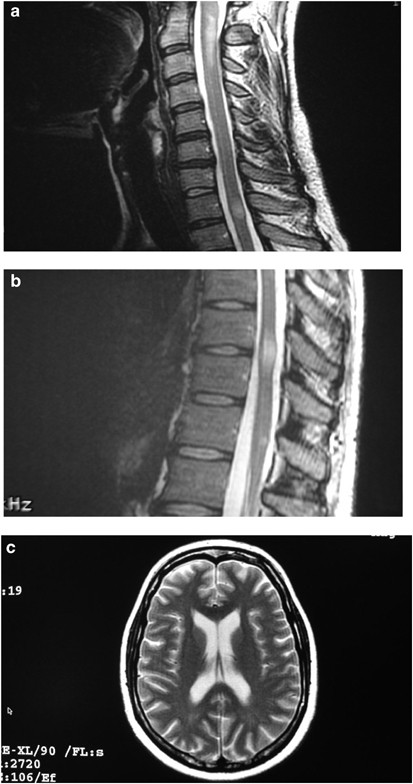
Imaging in multiple sclerosis | Journal of Neurology, Neurosurgery & PsychiatryLog in using your username and password Main menu Log in using your username and password You are hereArticle TextStatistics of Altmetric.com Suspected cases of multiple sclerosis (MS) are usually young adults attending the outpatient neurology clinic. The initiation of symptoms is rare before puberty or after 60 years; however, being a relatively common neurological disease (1:800 in the United Kingdom), both situations may be familiar with practicing neurologists. A normal MRI is usually presented with a history of acute relapse or with progressive neurological impairment MS key points is a clinical diagnosisThe effectiveness of the research can only be extrapolated from a clinical insulated study if the clinical picture is the same as in the studyBone magnetic resonance is abnormal in most patients with MSPatients with a single-phase presentation can be diagnosed with progressive MCBer interval RELAPSING REMITING DISEASE MS's most common presentation is following a relapse. The maximum age of the first episode is in the third decade; however, patients usually present the neurologist later with their second or third relapse or less commonly in the secondary progressive phase of the disease. This form of MS is twice more common in women than in men. The most common scenario is a 20 to 40-year-old patient who urgently refers to the outpatient clinic with a sub-accessive appearance of neurological disturbances, more commonly sensory symptoms, often solving for the time they are seen. Because sensory symptoms may occur in the absence of clinical signs, the neurological examination may be normal or almost normal even when observed during relapse. The distribution of sensory loss is extremely variable but most commonly implies one or more extremities and usually represents a partial cross-sectional myelitis with an evolving sensory level (which can be patch or unilateral). Optical neuritis is also common but usually presents the ophthalmology department. Other common presentations include more extensive cross-sectional myelitis with the involvement of the motor and bladder, symptoms of stroke including the diplopia (usually an internuclear ophthalmoplegia), alteration of the cerebello and the vestibular, and the phenomenon of Lhermitte. Less frequent but more specific are symptoms such as the Uhthoff phenomenon (the original description is symptoms induced by reversible exercise, now more commonly referred to as symptoms induced by heat), and paroxysmal stereotypical symptoms occur many times a day for seconds at a time during a relapse time course. The latter may imply the dysonic position of a member or side of the body. Fatigue and cognitive disturbance may occur less frequently along with other symptoms but are rare as isolated presentations. A relapse has been defined for clinical trials that last at least 24 hours in the context of a normal body temperature. It has been suggested that a 30-day period should separate the start of two events to be documented as separate attacks. The most typical time course is that symptoms evolve for days to two weeks, stabilize for 1–2 weeks and then improve for weeks. Partial recovery with persistent residual symptoms and longer recovery periods can occur, especially with more severe relapses. The outpatient clinic of neurology is full of people with a history of episodic neurological symptoms, particularly sensory disturbances. The decision to investigate will depend on the specificity of the symptoms for the EM, that is, a reasonable distribution of the sensory symptoms, maximal over a course of relapse time, and that may be associated with other suggestive complaints. Poly-sytomatic patients with normal neurological examination should not be investigated primarily for the possibility of MS. Fatigue is another unspecific common symptom seen in the neurological clinic environment. The fatigue of the type "MS" differs from the fatigue associated with depression in which it is associated with specific neurological symptoms, fluctuates with heat, exercise or when the day proceeds, and relieves itself for a short period of rest. Fatigue associated with depression tends to be described as a non-specific lack of energy and may be associated with other depression features, such as sleep disturbance. However, depression also commonly coexists in patients with organic disorders such as MS. Currently many neurologists along with their patients prefer not to investigate a single attack solved, especially when no objective signs have been observed. However, if it is shown that early treatment with modification of the therapies for the disease reduces long-term disability to a clinically useful degree, then the threshold for early patient research will be reduced. Abbreviations Primary progressive disease The progressive primary form of MS (which is found in about 10% of MS patients) has an insidious and vague beginning, which often precedes the referral to a neurologist for several years. It is not only the age of beginning later than with the form of relapse of remittances (which means about 40 years), but it is the most common form in older persons. The presentation of the progressive disease can represent the primary or secondary progressive MS, the second one is not infrequently associated with one or two, often misrepresented, relapsed many years earlier. Primary progressive MS usually presents the outpatient neurology clinic with a request to evaluate a progressive gait disorder. Patients may underestimate their neurological deterioration due to the slow deterioration of their walking, allowing them to adapt to maintain functional capacity. Patients and their general practitioners often put the initial symptoms to "age" or "arthritis". By the time they are examined by a neurologist, the test is often evidently abnormal with pyramidal dysfunction of the lower extremity. Ataxia is also seen frequently. This presentation clearly contrasts with the relapse of the remission. What research are available to help support the diagnosis of MS? There are three main researches that, due to their high specificity and sensitivity, are valuable in the diagnosis of MS: magnetic resonance (MRI), evoked potentials; and cerebrospinal fluid (CSF) examination for the presence of oligo-cellal bands (OCBs). MAGNETIC RESONANCE IMAGINGT2 weighted brain MRI is abnormal in about 95% of patients with clinically defined MS. The white matter lesions (WMLs) observed in such image correlate well with pathologically macroscopic plates. Although MMMs are seen in other conditions, the most frequent difference is ischemic and age-related changes. The useful distinction characteristics are set out in the table. Although these improvements improve the specificity of the EM, MRI is not a pathologically definitive research; also up to 4% of normal healthy controls have indistinguishable periventricular lesions of the MS and the precaution should be exercised in the use of MRI only to diagnose the EM, especially in patients with atypical or non-specific stories. In these circumstances, a typical MRI MRI resonance with a neuroradiologist and an additional clinical assessment or additional research considered is needed. Characteristics that distinguish multiple sclerosis from causes related to age and vascular causes in the magnetic resonance of the brain is often less abnormal in primary progressive MS, possibly as a result of a pathology of the spinal cord and/or a different pathological spectrum (i.e. a more widespread axonopathy). Ice enhancement is observed with new early active lesions due to the breakdown of the blood cerebral barrier, and usually lasts 4-6 weeks. The increase of the ring and the effect of mass with acute lesions can be observed. The new activity of improvement of the lesion is 5 to 10 times more frequent than the frequency of clinical relapse, so the tendency to implement this technique as a result measure that has been supplemented in clinical trials. Routine use of contrast is expensive and requires the need for patient cannulation. In fact, the improved image of gadolinium rarely adds much useful information in clinical practice, except when it differs from diseases that have associated meningeal inflammation, such as sarcoidosis. The demonstration of improving the lesions six months after a monophasic disease indicates spatial and temporal spread, but most doctors still prefer more clinical evidence before making a definitive diagnosis. Spinal cord injuries are common in the MS and their detection is useful as a diagnostic tool in older patients. MS occasionally coexists with the compression of the spinal cord, and spinal cord lesions are usually located near the compression site. In patients with progressive symptoms of lower limbs it is important but often difficult to distinguish between intrinsic ischemic changes associated anatomically caused by the compression of inflammatory demysyllation. As a general rule, MS lesions tend to be at a higher level while intrinsic ischemic compression lesions are located at the highest compression site. When brain MRI is used as diagnostic criteria for research studies, the need for specificity predominates on sensitivity, and therefore more stringent criteria have been suggested including three, four or eight LMAs, lesions greater than 3 mm or 6 mm in diameter, and several combinations of characteristics as set out in the table. EVOKED POTENTIALS The driving rate and the amplitude of the nervous impulse (from the stimulus site to the cortex) of the later visual, auditory, sensory column and engine systems (cortex to muscle) can be measured using evoked potentials. Of these visual evocados (VEPs) contribute more to the diagnosis of MS. The delay is indicative of the demystification in the visual pathways. The reduction of the amplitude can occur secondary to driving block and dispersion, as well as axonal damage, an important determinant of disability in the EM. Using evoked potentials you can determine the level of initial delay or block, but no more proximal sites of damage in number or position can be identified. It may be for this reason that although the possibilities evoked are more easily quantifiable than MRI their use in monitoring the effectiveness of treatment tests has been limited. EVOCADOS VISALES. Although the long-term conversion rate reports of optical neuritis to MS vary enormously, optical nerve involvement (even in the absence of a clinical episode) is extremely common in MS. Therefore, the evaluation of the visual system, in particular the previous pathways, is useful. The frequency of abnormal VEPs in patients with clinically defined MS varies between studies of 42 to 100% and is likely to depend on the time of occurrence of diseases when tested. A delay in P100 (higher positive deflection that occurs at about 100 ms using the pattern reversal technique) is the typical anomaly that incites demitation. However, asymmetry of delays between the sides of more than 6 ms and central stimulation tests can increase the sensitivity to the lesions of the optical nerve. During the acute phase of optic neuritis the amplitude can be reduced or absent if the visual acuity is less than 6/24. PEPs are more sensitive than detailed clinical tests, including field mapping and color desaturation tests, and examination of optical funds and pupil responses. In addition to sensitivity, the utility of VEPs arises from the persistence of abnormality with the clinical recovery of optical neuritis (80-90%), or even in the absence of a clinical event that marks a clinically silent injury. However, the growing age, lack of attention, drowsiness and optic nerve compression also increase latency. In patients with ocular disease that cause a central scotoma, PEPs that emerge from paramacular regions will produce an increase in latency. Refractive errors should be corrected when possible. Abnormal VEPs may occasionally occur in other conditions such as hereditary ataxias, B12 deficiency, neurosyphilis, Parkinson disease and metabolic alterations. However, these disorders tend to cause symmetrical abnormalities. The lesions of the posterior visual pathway can be identified by medium-field stimulation. EVOCADOS POTENTIALES OF SOMATOSENSORYAfter applying a brief electrical stimulus to medium or later tibial nerves, recordings are made at various levels that end in the primary somatosensor cortex. The peripheral component is restricted to obtain a central driving measure. Abnormalities of sensory evoked potentials have been reported in about 80% of patients with clinically defined MS, many of whom do not have relevant symptoms. Metabolic disorders such as B12 deficiency and focal lesions that affect the somatosensible pathway can interrupt driving. BRAINSTEM AUDITORY EVOKED POTENTIALS This measures five waves of short-latence response from the moment of hearing stimulation to the upper olive complex, the lateral lemnisco and the lower colliculus. This test is omitted in a potential screen evoked by many centers due to its less sensitivity in MS. It is also not specific to MS and detects mid- pontine/low brain injuries resulting from other causes. Brainstem's evoked hearing potentials require more technical experience than other potentials evoked to deliver reliable results. As with the other evoked potentials, organ damage may interfere with the response. MAGNETICALLY EVOKED MOTOR POTENTIALS. A short and powerful magnetic stimulus is applied to the scalp over the region of the primary motor cortex on both sides. This produces an electrical current in the underlying cerebral cortex and causes primary motor neurons to be discharged. Recordings of distal magnetic evocation potential are made. This test is of low specificity—which deteriorates in a wide range of other neurological disorders—and reports of its sensitivity, especially in the absence of a clinically relevant lesion, vary. CEREBROSPINAL FLUID EXAMINATIONOligoclonal bands The oligoclonal band in the CSF does not match in the serum has high specificity and sensitivity for MS, although the first depends on the differential diagnoses considered. About 95% of patients with clinically defined MS have OCBs by isoelectric approach. It is well recognized that many inflammatory diseases can be CSF OCB positive. In addition, it has been observed that about 4% of patients with non-inflammatory neurological diagnosis produce OCB in the CSF. OCB patterns are notably stable within an individual with MS for many years, although absolute concentrations of IgG may decrease. This observation supports the OCBs as representing a specific immune reaction within the CSF rather than a non-specific effect of supporting. Other CSF components The protein is usually normal but can be raised minimally. The slightly elevated lymphocyte counts are common but it is rare that this exceeds 50 cells/mm3. High neutrophil counts are not seen in MS (but may be found in Devic's disease). Cell counting and other specific CSF tests can be useful for differentiating between MS and other inflammatory diseases of the central nervous system. How is the diagnosis of MS done? It should be noted that the diagnosis of relapse of MS (fig) remission is mainly a clinical one and therefore the investigation must follow a suspicious record. Because the MRI can show abnormalities in healthy controls, testing to rule out the diagnosis can be misleading and can make it difficult to manage later. In addition, all investigations have a false negative rate. The diagnosis of MS is based on the clinical (and paraclinic) evidence of typical injuries/events spread in time and place. The safety of each clinical attack as a MS relapse depends on the pattern and distribution of symptoms and previous documentation of objective signs. In 1983, a committee developed diagnostic criteria for MS, the degree of certainty dependent on MS relapse evidence, research that reveals clinically silent lesions and CSF OCBs. Using such criteria of Poser (Table) the specificity for clinically defined MS is 94%. These criteria have been updated recently, incorporating the use of MRI to ensure diagnosis in mono-synthmatic situations (Table) and simplifying diagnostic categories in "MS", "not MS", and "possible MS". Flow chart showing the stages in the diagnosis of multiple sclerosis (MS) leading to a confirmed diagnosis. CSF, cerebrospinal fluid; EPs, evoked potentials; MRI, MRI. Poser criteria for diagnosis of clinically defined multiple sclerosis (MS) and MS-compatible laboratory (Poser et al6 models)Recently proposed diagnostic criteria for multiple sclerosis (McDonald et al1)PRESENTATION WITH A SECOND CLINIC RELAPSO OR MORE This is the most direct situation. When a 20-30-year-old patient has a second typical neurological episode supported by a characteristic brain resonance feature, most doctors would feel confident enough to tell the patient that they have MS (even when they have not been seen and examined during the first attack). Other tests help identify the small number of patients with EM in which brain MRI is negative or border. Evoked potentials can identify additional paraclinical lesions in such circumstances, and the typical anomalies of the CSF exam and the cerebral MRI cannot always coexist, so lumbar puncture can increase diagnostic certainty. SUBMISSION IN THE FIRST EPISODEA Clinic only clinical episode is insufficient for the diagnosis of the clinically defined EM. However, the laboratory diagnosis supported defined MS, includes patients with monophase clinical presentations in the presence of CSF OCBs and evidence of two or more lesions. About 60% of patients with a typical isolated clinical syndrome of type "MS" will have multiple white matter (asymptomatic) lesions in magnetic resonance. The presence of an abnormal brain MRI (one or more typical asymptomatic lesion) in this clinical environment is associated with a risk of 83% of developing a clinically defined EMS after 10 years. The longer follow-up periods and longitudinal studies of the MRI and/or evoked potentials can increase this figure. Updated guidelines allow for a diagnosis of MS in patients where longitudinal research shows evidence of new lesions in the MRI. If one defines a brain resonance as "abnormal" when there are some number of defined lesions of white matter, this research seems to be more sensitive than the evoked potentials and the CSF to predict which patients develop MS in follow-up. Increase the degrees of abnormality, such as the number of lesions, does not increase the sensitivity to conversion rates for 10 years, but rather predicts a worse disability (to 5 and 10 years of follow-up) and once more early to conversion. Therefore, in the clinical environment, the brain MRI can indicate how likely it is that a patient with a single typical neurological episode advances to the MS clinically defined in the future, and now longitudinal studies have been promoted to make the diagnosis. A negative scan can provide some reassurance, only 11% of these patients developed clinically defined MS for 10 years. However, these MRI data can only be extracted and used prognostically if the clinical picture is as safe as in the original study. INTRODUCTION WITH A PROGRAPHIC PICTURE Diagnosis in patients with progressive problems should only be done after other causes are discarded: in particular the compression of the spinal cord and other structural lesions of the spinal cord and brain. Other rarer differential diagnoses should be considered as appropriate and include: inflammatory conditions involving the central nervous system (e.g., systemic erythematous lupus, Sjogrens syndrome, sarcoidosis); combined subacute degeneration of the cord, infection (e.g., syphilis, HTLV-1); neuron motor disease in the absence of minor pneumotic abnormalities, and lower motor neuronate conditions). Due to the delay in the introduction to a neurologist in the progressive primary EM, the clinical picture of progressive deterioration is generally clear. Due to the previous age in the presentation, a greater proportion of patients will present after the age of 50 and the usual confirmed cerebral MRI appearances can be difficult to distinguish from the related and commonly seen MRIs. The addition of the spinal cord MRI contributes enormously to the research of such patients, not only because it is useful to eliminate other important differential diagnoses, but because spinal cord injuries are commonly seen in the MS. In fact, a series found spinal cord injuries in all negative patients of the cerebral RRM. In contrast, by-carriage lesions of the spinal cord are rare and are not presented as a characteristic related to age. Thus, patients who are researched with a progressive primary form of MS are more likely to require spinal cord MRI, CSF examination and potential evoked to establish the diagnosis, than patients who present a relapse pattern of the remission. INITIAL INVESTIGATIONS Normal brain RRM is found in only 5% of patients with MS using modern techniques. Half of the patients in a series consisted of patients with progressive primary disease, most of whom were severely disabled. As remittance disease fell, the normal image was associated with early or mild disease. All negative patients with cerebral MRI had at least one spinal cord injury using modern imaging techniques, 87% had ECB and 56% abnormal VEP showing the added value of these additional research. The complete normality of the three investigations (when optimal techniques are used) would seriously question the diagnosis of MS. In patients with relapsed symptoms most have no objective signs and a non-organic diagnosis is the most common conclusion. However, a minority of patients with early relapse (often monophasic) symptoms that are initially negative in research continue to develop new problems and show abnormalities in repeated research. In patients with alternative diagnosis of progressive disease should be considered. What other diagnoses should be considered? The differential diagnosis of MS is discussed in detail in other places (see article by the scolours in p ii9). Where appropriate, a number of these conditions must be ruled out. Discuss the diagnosis of MS with the patient INITIALLY IN THE OUTPATIENT CLINIC The objectives when the diagnosis of MS is initially discussed are to reduce the initial shock when the term MS is first used and give an optimistic picture of the forecast. MS patient perception is usually worse than reality unless you have personal experience of someone with mild disease. Discuss the possibility of diagnosis (together with other possible suggestions—i.e., "a viral disease", "do not find an explanatory cause") in the initial consultation, when the clinical picture is suggestive but before the investigations, it takes the patient more carefully to the MS label. This approach can increase the anxiety of susceptible people while awaiting research and follow-up on appointments. In addition, anxiety can be unnecessary, so the patient's personality and degree of clinical suspicion must be taken into account. Breaking news for the patient is best done in the presence of a partner, friend or family member, and it is easier to ask someone to attend with them in follow-up if the MS possibility has already been elevated. Inevitably MS will be discussed at the time the diagnosis is confirmed, many questions addressed by the patient and the companion, especially if it was predicted about the possible diagnosis. Many centers have access to a MS nurse and patients are grateful to receive a contact number at an early stage. A good communication of prior conversations with the patient along with the corresponding letters must be sent to the nurse. It is preferable to arrange for the MS nurse to be present at the clinic (by allowing them to capture the situation well and an initial rapport) that can organize an additional follow-up session with the patient. Follow us at the session Most of the patients and their families (who often have as many questions as the patient) find a welcome formal orientation/education session. It is useful to give an interval of the initial consultation of neurology to allow them to collect their thoughts and write their questions once the diagnosis has sunk. Many patients find that the unpredictability of the MS difficult to cope with or prepare for additional sessions and may be necessary, especially when the level of anxiety is high. The availability of a telephone line is also very reassuring and used with great variability. In many patients the emotional reaction is more deactivating for the patient than the MS, and this is especially true in the first two years of diagnosis. FOLLOW US ON NEUROLOGY When patients are seen during an unsolved relapse or in the progressive phase of the disease, it is reassuring that they are given an additional appointment to see the neurologist. Although it is not possible to follow all patients with chronic neurological disease, early support while reaching terms with the diagnosis may prevent the interpretation of the disinterest that patients sometimes attribute to their consultant. References Request for permissions If you wish to reuse any or all of this article, please use the link below that will take you to the RightsLink Service of the Copyright Settlement Center. You will be able to get a quick price and instant permission to reuse the content in many different ways. Copyright Information: Read the full text or download the PDF: Sign in using your username and password Online: ISSN 1468-330XPrint: ISSN 0022-3050 Copyright © 2021 BMJ Publishing Group Ltd. All rights reserved. 4.00ICP sponsors15042040 forwarded-3
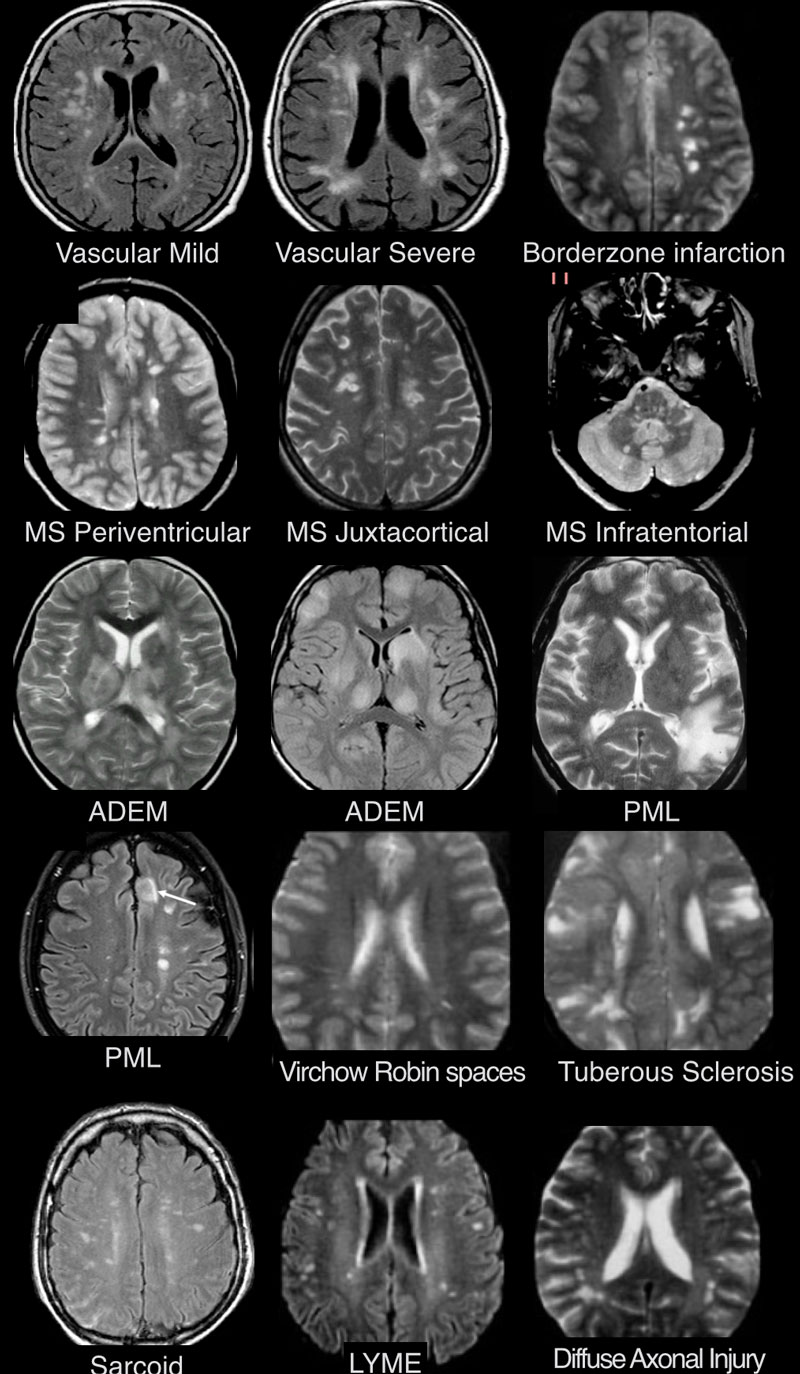
The Radiology Assistant : Multiple Sclerosis - Diagnosis and differential diagnosis

Differentiating Multiple Sclerosis Mimics on MRI - Neurology Advisor
Multiple Sclerosis
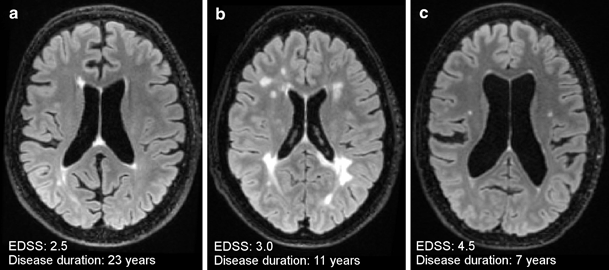
MRI in the Diagnosis and Monitoring of Multiple Sclerosis: An Update | SpringerLink

MRI Uses in MS - YouTube

Imaging in multiple sclerosis | Journal of Neurology, Neurosurgery & Psychiatry

The Radiology Assistant : Multiple Sclerosis - Diagnosis and differential diagnosis

Differential diagnosis of multiple sclerosis and other inflammatory CNS diseases - Multiple Sclerosis and Related Disorders

Diagnosis and Management of Multiple Sclerosis - American Family Physician
MS Advanced Course

Multiple Sclerosis Foundation - 5 Things to Know About MRIs and MS
Multiple sclerosis - Diagnosis and treatment - Mayo Clinic
The Radiology Assistant : Multiple Sclerosis - Diagnosis and differential diagnosis

New MRI Finding Sheds Light on Multiple Sclerosis Disease Progression

MRI and MS: 7 things you need to know | Multiple Sclerosis Society UK
MS Composite

Non-contrast MRI is effective in monitoring multiple sclerosis patients
MS brain lesions: Pictures and prognosis
MS Explained - Brain Lesions and More

Multiple Sclerosis in the Very Young – Consult QD

MS and dizziness

Spinal cord abnormalities in recently diagnosed MS patients | Neurology
MS Brain Lesions: Pictures, Symptoms, and More
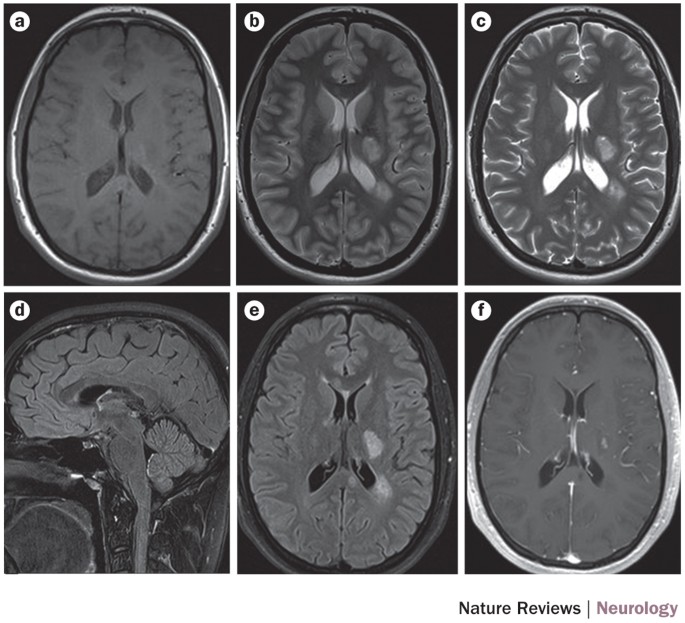
MAGNIMS consensus guidelines on the use of MRI in multiple sclerosis—clinical implementation in the diagnostic process | Nature Reviews Neurology

The Radiology Assistant : Multiple Sclerosis - Diagnosis and differential diagnosis
The Multiple Sclerosis Lesion Checklist - Practical Neurology

MRI Brain With Contrast Multiple Sclerosis | Mri Scan Images | Mri brain, Multiple sclerosis awareness, Multiple sclerosis

Magnetic resonance imaging in primary progressive multiple sclerosis

Multiple Sclerosis | NEJM
/what-are-these-spots-on-my-mri-2488902-5c5db0fa46e0fb0001ca86cb.png)
Spots on an MRI: White Matter Hyperintensities

Non-contrast MRI is effective in monitoring multiple sclerosis patients

Multiple Sclerosis (MS) - Neurologic Disorders - Merck Manuals Professional Edition
The Multiple Sclerosis Lesion Checklist - Practical Neurology

Multiple Sclerosis: When to Suspect—Keys to Diagnosis | Consultant360
Need to Know: Do I Need Contrast Dye for an MRI?

What Tests Are There for Diagnosing MS?

His Symptoms Pointed to M.S. Then He Had a Strange Personality Shift. - The New York Times
Clinical characteristics, course and prognosis of spinal multiple sclerosis | Spinal Cord
/lupus-and-ms-whats-the-difference-2249979-v2-5c45534dc9e77c000163bb17.png)
Differences Between Lupus and MS

MAKING THE DIAGNOSIS OF MULTIPLE SCLEROSIS | Journal of Neurology, Neurosurgery & Psychiatry
Posting Komentar untuk "ms symptoms but normal mri"